THE HEALTHCARE PLAY SPECIALIST EDUCATION TRUST (HPSET) – A HISTORY
INTRODUCTION
HPSET as we know it now has come from a long and interesting journey. This background history catalogues the need for a separate registration body for the training support, the registration and maintenance of professional standards of Healthcare Play Specialists.
This responsibility has sat with the Educational Trust since 1985, with the intent of national recognition. The chronology in section two follows a record of key moments in the development of hospital play over that time.
This is taken from my own recollection and my archivist records I previously gathered for the National Association of Healthcare Play Specialists (NAHPS) out of which the HPSET Board was formed. I also have papers belonging to Susan Harvey that were left with me. I have given the background of the two associations because HPSET was formed out of NAHPS and thus their histories are intertwined.
I am very grateful to my fellow trustee Janet Morris who has worked with me on this. This would also not have been possible without the contribution of others, with memories, stories, photographs and historic publications.
Our aim, as a Board, is that this will serve as a resource for students and colleagues alike and will continue to grow as a record of the ongoing exciting journey of this specialty so that those of us who remain with the passion will not forget that the Trust was formed with the sole intention of achieving the necessary national registration status for healthcare play specialists which is the right thing for children.
Judy Dibble
BACKGROUND TO THE FORMATION OF HPSET IN 1985
1985
 Figure 1. Susan Harvey (right) with Yvonny Lindquist (center) and Viv Harding
Figure 1. Susan Harvey (right) with Yvonny Lindquist (center) and Viv Harding
Hospital play as we know it was founded on Susan Harvey’s enthusiasm. Susan was a Froebel trained teacher and met Dr. David Morris at a conference in South America. This was organised by the world organisation for early childhood education (OMEP). The abbreviation is derived from the French title ‘Organisation Mondiale pour L’Education Prescolaire’. Susan was instrumental in enlarging the network of professionals interested in hospital play, meeting with David and other professionals at conferences in the United Kingdom and internationally and communicating globally with like- minded people. In Sweden Yvonny Lindquist, a hospital teacher, became a staunch supporter and shared her experiences of Swedish practice on children’s wards. Yvonny had also published articles and books on Play for Children.
OMEP UK agreed to set up a working party on the value of play for the sick child. As a result ‘The Play in Hospital’ booklet was later produced (in 1966) with recommendations by the ‘National Committee of OMEP’. It stated that imaginative play schemes should be provided in all children’s wards: “This work should be under the supervision of trained and experienced people and every opportunity should be taken to encourage understanding of the importance of children’s play by the medical and nursing staff”.
 Figure 1. Susan Harvey (right) with Yvonny Lindquist (center) and Viv Harding
Figure 1. Susan Harvey (right) with Yvonny Lindquist (center) and Viv Harding Figure 2. First SCF Play Worker – Gabi Marston (Brook Hospital)
Figure 2. First SCF Play Worker – Gabi Marston (Brook Hospital)In 1963 Susan Harvey, who had previously worked for the charity Save the Children Fund (SCF) as a senior play advisor, approached the SCF charity to fund a hospital play scheme. The Brook Hospital, Greenwich, was chosen as the first site and the first SCF Play Leader was appointed. SCF employed Susan as the hospital play advisor for the project. Following this there was a slow but steady expansion of hospital play schemes throughout England (over many years). The SCF charitable funding provided Hospital based staff with external advisors employed to visit and support.
 Figure 3. World Medicine Vol. 1 No. 7: Lady Green at Barts plays with a child while Sister Kenton administers treatment
Figure 3. World Medicine Vol. 1 No. 7: Lady Green at Barts plays with a child while Sister Kenton administers treatmentSeparately, five years earlier (in 1958), the Governors of St Bartholomew’s Hospital made the decision to appoint a ‘Lady Green’ (the name originating from the green overall to differentiate from the nursing staff).
The role was to play with children on their two children’s wards (Kenton and Lucas). The first Lady Green who started the play scheme was teacher trained and thereafter the Lady Green in post would be Norland trained. This post is still current.
 Figure 4. My acting skills but I list my voice with the stress!
Figure 4. My acting skills but I list my voice with the stress!
 Figure 5. The answer
Figure 5. The answer
The Governors of the hospital, keen to promote play for the children on the wards, suggested I (as the Lady Green in 1960) should go on a popular TV programme at the time ‘What’s My Line’.
I acted out an activity of my work to a panel who then asked questions trying to identify my job.
Lady Isobel Barnett, a doctor, guessed at the 8th of 10 possible tries but said she had not heard of the particular role. Lots of enquiries followed which showed that St. Bartholomew’s had successfully promoted the work.
Over the next 20 years (until the formation of HPSET in 1985), as SCF posts were coming into being, there was also an increasingly wider focus on the plight of hospitalised children, regarding their welfare and needs. Several reports were compiled over this time and play for children in hospital, tailored to their particular experience, became one of the facets seen increasingly as essential.
The Play in Hospital Liaison Committee (PHLC) was formed in 1971, bringing together interested professionals and bodies. Their aim was to promote the appointment of playworkers. This committee devised surveys, organised conferences and produced publications.
In 1975 Susan Harvey drew together a group of interested professionals from around the UK. Some were working as play staff in hospitals and I was one of those and attended the first meeting. This group formed into the National Association of Hospital Play Staff (NAHPS) with Susan as the first Chair. The first meetings were held at the Thomas Coram Playgroup and subsequently at the Thomas Coram Children’s Centre, Brunswick Square.
 Figure 6. Dr Hugh Jolly
Figure 6. Dr Hugh JollyThe need for formal training of the hospital play staff specific to this work, was recognised by the early 1970’s and, in 1973, Susan Harvey established the first training course at Chiswick Polytechnic (later, in 1978, transferring to Southwark College). Dr Hugh Jolly, Consultant Paediatrician, a strong advocate for the provision of play for hospitalised children, advised on the setting up of this course and was appointed as the external examiner of the special studies. Three more Colleges subsequently delivered courses with the appointment of local paediatricians informed by Dr Jolly.
College tutors formed a group together from each course so that they could discuss assessment, syllabus and share local and cultural differences. This group of educationalists were evidencing the need for an educational body serving NAHPS, to register the training of hospital play staff. I recall, as a play specialist tutor, how invaluable we found the interaction with the now formed Board. Membership of this group of tutors increased as more Colleges came on board and when I later joined the Board (as a representative of NAHPS) I witnessed the interface that had shaped the hospital play specialist training and influenced the tasks of the Board, in order for it to become the registration body for hospital play specialism.
 Figure 7. Dr David Morris delivering the Hugh Jolly lecture 1988
Figure 7. Dr David Morris delivering the Hugh Jolly lecture 1988Dr David Morris, a strong proponent of play for children in hospital, realised that many play staff were the only one of their kind working in isolation. Throughout this time he supported us, initially hosting support meetings in his home. Minutes of these meetings from 1969 indicate that, on a monthly basis, play staff were given the opportunity to share experiences and to present a case or problem to the group. They also reflect the lively discussion and the supportive ambience of these meetings. NAHPS branches were formed in different parts of the UK to share and support and Executive Members of NAHPS visited regularly reporting back on discussion items.
In March 1976 the DHSS had produced a health circular that strongly recommended that hospitals where children are admitted as patients should recognise their need for play and make the best arrangements possible, within the limits of existing resources to meet this need. These recommendations came from the appointed Expert Group in Play for Children in Hospital. Susan Harvey was appointed a member of this panel in 1972. The report, in its summary of recommendations and conclusions, stated that :
“the nature of the work involved and existing workload on nursing staff make it unrealistic to expect nurses employed as such to take total responsibility for developing play.”
An addendum was made to this report that had proposed the creation of a new profession- the playworker. The addendum stated that:
“Although the proposition about a new profession could be reconsidered in the future in the light of further experience there are recent and prospective developments in the nurse training field since the Expert Group studied the question, which should make it increasingly possible for nursing staff to include play in the care they provide for their child patients, and thus help meet the Expert Group’s recommendations.”
I recall detailed discussion at the time at an open meeting of NAHPS that this was at odds with the Expert Group’s recommendations. This was pointed out to the meeting by members of the expert group.
Also in 1976, the Department of Health and Social Security (DHSS) Report of a Committee of the Central Health Services Council ‘The Organisation of the Inpatient Day’ was published. In the section ‘Play and Education’ it reads:
“It is recommended that hospitals employ professionally trained playworkers specifically designated as a separate group of hospital staff. Certain groups of children are in particular need of organised play. These include long stay children, children who are not visited, children in isolation wards, children with sensory loss, severely ill children and children recovering from the distress of operations and other emergencies. Not all hospitals have teachers or children of school age. There is a need for Area Health Authorities to review their arrangements in discussion with local Education Authorities to make good the deficiency.”
A separate Consumers Association report produced in 1979 (activated by a parent who had experienced having a child in hospital) focused on a review twenty years on from the Platt report (DHSS report ‘The Welfare of Children in Hospital’ 1959 – the year a Lady Green was first appointed!). The Consumer Association report echoed the message of the Platt report and the later Court report (1976), with recommendations for more trained paediatric nurses and more playworkers but it also indicated that there was a great deal of thinking to be done about the organisational factors of ward life which causes emotional stress in children over and above that caused by the presence or absence of parents. However the Consumer Association focus was on parents and organisation. To quote the report:
“There is much to be done to re-think care assignment rather than task assignment on wards. There needs to be more careful thinking too in defining the parent’s role on the ward so that they do not become bored and wish they were not there.”
A clear and supportive policy paper was adopted by NAWCH (The National Association for the Welfare of Children in Hospital) in 1985. This set out their ‘Play in Hospital’ beliefs.
In 1990, the publication ’Setting Standards for Adolescents in Hospital’ (NAWCH), stated that adolescents have distinct needs which are very different from adults and small children. Under the heading play/recreation it states:
“Specialist play/recreation are essential for the equilibrium of the unit and often have a therapeutic and counselling role among adolescents. Play specialists have an important role in providing an appropriate atmosphere for adolescents. They can ensure that relevant information is available and that other staff are aware of the adolescent’s needs for privacy and independence. They should encourage group activities and encourage patients to meet each other, share experiences and anxieties as well as their own methods of coping with hospital life”.
Save the Children Fund in 1989 published ‘Hospital: A Deprived Environment for Children?’ This publication had a foreword by Dr David Harvey, Consultant Paediatrician:
“When I was a junior Doctor at Great Ormond Street, I first met play specialists from SCF and later when I became a Consultant at St. Charles Hospital, I was very proud that SCF had a playgroup there. It did not take long to convince me that play had a lot to offer ill children. There are many deprived inner city areas in Britain; some of the children living there have never had much chance to play and a playgroup in hospital gives them their first chance, as well as filling in empty hours on the ward. Play has much to offer the medical team, I can remember a child who was partially blind and this was discovered by the play specialist from some paintings. Many children have given us valuable clues to their emotional life from pictures they have drawn. There are many areas in which I should like play to develop and we could do so much more for teenagers on our wards. This document sets out the strong case for hospital play schemes. I hope that lessons from the document will be learnt well and supported enthusiastically.”
The chapters cover the theories of play, effects of hospitalisation, play in hospital, role and training of the play specialist, SCF and hospital play schemes, developing SCF’s role, and (in the summary) the handing over of established play schemes to the hospitals wherever possible.
 |
 |
| Figure 8. Dr David Harvey delivers the first Hugh Jolly lecture. Mrs Peg Belson (right), a Patron of NAHPS. | Figure 9. Dr David Harvey, VICE President NAHPS |
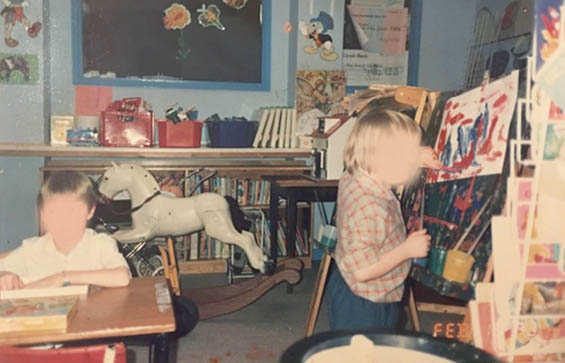
Play Activities in Hospital
 |
 |
 |
| Figure 10. Hospital rabbit | Figure 11. Painting and puzzles | Figure 12. Eve Latimer – reading – at Whittington Hospital |
 |
 |
 |
| Figure 13. Sand play | Figure 14. Breathing checks | Figure 15. Bathing dolly – in isolation |
 |
 |
|
| Figure 16. Judy Walker – doll play insertion of a cannula | Figure 17. Francis Binns’ puppetry |
CHRONOLOGY OF HPSET SINCE 1985
1985
By January 1985 the Executive committee of the National Association of Hospital Play Staff (NAHPS) was preparing the ground
for the setting up of an Examination Board, to be organised by and to operate under the supervision of an independent charitable trust to be called ‘the hospital play staff education trust (HPSET)’.
 Figure 18. Susan Harvey (left) and Pam Barnes sign certificates for the first graduates 1988
Figure 18. Susan Harvey (left) and Pam Barnes sign certificates for the first graduates 1988On 15.1.85 an Extraordinary Meeting of NAHPS members was held, on the advice of solicitors Jacques & Lewis of Grays Inn to obtain formal approval to proposals to set up the Board.
The Declaration of Trust of the Hospital Play Staff Education Trust was submitted to the Charity Commission.
In October 1985 a grant was given from the Kings Fund to set up the Board. These monies were mistakenly given to the Board rather than the NAHPS Executive (the two were often mistaken for one another). The Department of Health in February 1989 awarded NAHPS a grant of £10,000, which was used to buy a new computer, so both grants were used to achieve the aims of NAHPS.
Representatives from various bodies concerned and involved in child health attended the first Board Meeting held on Tuesday 1st October 1985 at the Thomas Coram Foundation, Brunswick Square. NAHPS was invited to have three representatives.
The Examination Board wrote out its policies, aims and objectives and the duration and method of examination for courses.
1986
In 1986 the Hospital Play Staff Examination Board (HPSEB) set the syllabus, devised an examination paper
and appointed a chief examiner to scrutinize the examination papers.
1988
In 1988 the first certificates were signed by the Chief Examiner Susan Harvey and Chair Pamela Barnes.
Colleges now offering the hospital play course, called the Continuing Education Course (CEC), were:
- Southwark College
- Bilston College Wolverhampton
- Bolton College
- Stanmore College.
This course was a post qualifying course.
1992
In 1992 hospital play courses were advertised at:
- Basingstoke College of technology
- Bolton Metropolitan College
- Elm Park College Stanmore
- North East Surrey College of Technology at Reigate
- North Warwickshire College of Technology and Art
- Nursery Nurses College of Further Education, Bristol
- Southwark College
- Stevenson College Edinburgh
 Figure 19. Linda Weiss, Chair (right): celebrating DoH recognition of the profession with Patrons
Figure 19. Linda Weiss, Chair (right): celebrating DoH recognition of the profession with PatronsIn 1992 the qualification was recognised by the DoH (Department of Health) and DfEE (Department of Education and Employment). This huge achievement was celebrated on Thursday 22nd October. Lynda Weiss, Chair of NAHPS, said at the gathering in the play centre of Great Ormond Street:
“We want to celebrate our historic step forward. The Department of Health very seldom recognises a new profession and we decided to throw a party in honour of hospital play specialists everywhere.”
A career structure was drawn up by the NAHPS finance and general purposes committee and considered by the Department of Health.
Pamela Barnes wrote to Lynda Weiss, the NAHPS Chair, congratulating NAHPS on achieving a grading structure for hospital play specialists.
HPSET was approved as an awarding body by the Secretary of State for Education and the certificate received national recognition as the qualification for hospital play staff.
Following on from recognition in 1992 there was close collaboration with BTEC (Business and Technology Education Council/ Edexcel Foundation (Foundation for Educational Excellence). Students were assessed according to the regulations of BTEC and HPSEB.
Only students who had successfully completed the course through the Board /Trust and BTEC were eligible to register with HPSET as registered HPS’s.
1996
In January 1996 the Board reverted to its original title as it was no longer the Examining Body.
It had become the Registration Body and the Constitution was changed accordingly.
Two further awards were developed by 1997 the higher award (known as BTEC Professional Development Diploma In Hospital Play) and a self-development award (known as BTEC Professional Development Units for Updating Hospital Play Specialism).
Neither of these two awards was a qualification for registration. The qualification required to be a registered hospital play specialist remained the current course jointly endorsed by HPSET and BTEC/ Edexel i.e. the Professional Development Certificate in Hospital Play.
In 1996 the course was now delivered at:
- Bolton College
- Bristol College of Care and Early Education N.E. Surrey College of Technology, Epsom, Surrey.
- Southwark College, London.
- Stanmore College Middlesex Stevenson College Edinburgh
- North Warwickshire
- University of Hong Kong, with input from Hospital Play Specialists and Board members (the Board in an advisory capacity).
The two Colleges in Northern Ireland and Southern Ireland offered the course.
1997
In 1997 Approved courses for The Professional Certificate in Hospital Play were:
- Basford Hall College Child Health and Social Care, Nottingham
- Bolton College, Charles Keene College, Leicester
- City College, Norwich
- College of Care and Early Education, Bristol
- East Antrim Institute of Further and Higher Education, Newtownabbey, Co Antrim
- North East Surrey College of Technology (NESCOT), Epsom Surrey
- North Warwickshire and Hinkley College, Nuneaton, Warwickshire
- Preston College, Preston
- South Nottingham College, Science and Care Department, West Bridgford, Nottingham
- Southwark College, London
- Stanmore College Elm Park, Stanmore, Middlesex
- Stevenson College, Edinburgh
- Sutton Coalfield College, West Midlands The University of Hong Kong.
1998
In 1998 The Hospital Play Staff Education Trust ratified a policy on re-registration for Hospital Play Specialists.
Introduced in 2000, re-registration provided the qualified play specialist with the opportunity to demonstrate evidence of continued professional development based on updating knowledge and skills. Periodic re-registration is a valuable tool for maintaining the confidence of the public and other healthcare workers. The five yearly periodical programme of re-registration was based on the ‘PREP’ requirements operational within the nursing profession and was devised in accordance with the NHS Clinical Governance agenda. To reflect the scope of professional development opportunities available and to take account of changing needs of society (social, educational and economic) and the range of provision of child healthcare services the re-registration programme was fully revised and updated (in line with that used by The Health Professions Council).
With effect from January 2011 all healthcare play specialists were invited to re-register every two years from the date of initial registration or expiry date of current period of registration.
2004
In 2004, on the recommendation of the Board of Hospital Play Specialists Examination Board, the qualification was linked with
Business and Technology Education Council (B Tech) and EDEXEL. In 1995 a pilot course for a new BTEC qualification had been trailed at Bolton Community College, a new Level 4 qualification. A professional Diploma in specialised play for sick children and young people and this is accredited at Level 4 on the National Qualification Framework.
This level 4 qualification was intended for those who already held a professional childcare qualification and either wished to work or already worked within the National Health Service and would like to become hospital play specialists. Students had to have at least 3 years’ experience of working with children and be over 20 years of age at the commencement of the programme.
2006
In 2006 Approved programmes were:
- Bolton Community College, The City of Bristol College ( not running in 2006-2007 )
- East Antrim Institute
- Inchmore College Dublin
- Leicester College (not running in 2006-2007)
- North East Surrey College of Technology
- North Warwickshire and Hinckley College Nuneaton
- Preston College
- Stanmore College, Stevenson College Edinburgh.
- Southwark College
In 2006 the Declaration of Trust was registered with the Charity Commission for England and Wales (Charity no 292218), reviewing the first Declaration of Trust and the Deed of Variation, to enable Trust documentation to be updated. In the section [NAME] it states:
“Trustees may, by resolution, change the Charity’s name from time to time. Before doing this they must obtain the written approval of the Commission for the new name.”
2007
In 2007 (with the registration period for the Advanced Diploma in Specialised Play due to reach its expiry date)
a new course working party was set up by the Board to explore the future content and design of the qualification.
Learning from the difficulties experienced in implementing the Advanced Diploma there was an opportunity to develop a new programme of study leading to a professional qualification that fully encompassed the role of the hospital play specialist.
A robust consultation document was designed by the working party that was appointed by the Board. It was devised as an intention:
“to capture sufficient depth and breadth of evidence to give the Trustees a clear steer for the way forward. Respondents to the consultation were also invited to submit any additional information on a separate sheet. The high level of response received to the questionnaire was most encouraging and provided invaluable information to underpin the direction for the future development of the programme.”
Quote from the Chairman of the New Course Working Party.
The University of Shiozuoka in Japan received funding in 2007 from the Japanese Ministry of Education to train the first cohort of student Hospital Play Specialists in Japan, commencing in 2008. NAHPS and HPSET signed an agreement with the University of Shizuoka which supports the progression of play in hospital. Professor Makiko Tabu, Professor of Early Years Education in Japan was in London in 2012 to explore the training and work of the UK model of play specialism in contrast to the Japanese approach. Highly experienced Healthcare Play Specialists are invited to lecture on the programme in Japan.
2009
Throughout 2009 the focus was to develop and refine the Foundation Degree for the new programme of study in conjunction with
Thames Valley University, Stanmore College of Further Education and Bolton Community College.
The Further Education Colleges had been responsible for developing the academic material and HPSET had been responsible for developing the Practice Assessment Booklets.
Edexcel agreed to extend the course until December 2010.
2010
In March 2010 the external validation event for the new Foundation degree was held at Stanmore College.
Representatives from the Trustees of the HPSET Board were required to be present at the validation in order to answer any questions regarding placement outcomes/competences and to provide points of clarification from HPSET’s perspective.
Subject to three conditions and one recommendation approval was given to run the course. With confirmation by the University of West London that all three conditions and the recommendation had been met, enrolment of students at Stanmore College began on September 7th 2010. This go- ahead to run the course meant that marketing the programme, selecting students plus developing and delivering the mentor training was completed in a short time frame in readiness for the enrolment of students in September 2010.
With extensive consultation with HPSET, the qualification was designed to be fit for purpose in that it was:
- Able to meet the changing needs/ direction of Healthcare.
- Would be recognised as a qualification that stood alongside other qualifications that were regulated by The Health Professions Council.
The qualification moved to a Foundation Degree (FdA) in Healthcare Play Specialism with entry to the Professional Register at Level 5.
October 2010 saw the final tutors meeting (these regular meetings with a Tutor Representative reporting back to the HPSET Board meetings had taken place for over twenty years).
2012
In 2012 successful graduates in the Foundation degree graduated from Stanmore College.
Bolton College in January 2012 completed the first year of the Foundation degree.
2013
In 2013 North Warwickshire and Hinkley College was approved to offer the course by The University of West London.
Cardiff and Vale College enrolled students on the long awaited play specialism course to be run in Wales.
In 2014 these four Colleges were offering the course.
2016 Re-validation of the Foundation Degree in Healthcare Play Specialism by the University of West London was achieved. A rigorous quality review of the academic elements of the course resulted in revalidation for the next five years. It required re-writing of the competency handbook, meeting with mentor representatives, and a formal panel review including external experts.
In 2013 the title of the professional was changed by the National Association to Healthcare Play Specialist and the Board agreed to its new title ‘the Healthcare Play Specialist Education Trust (HPSET)’.
These changes reflected the changing role of the play specialist in the wider community.
In 2016 The FdA Healthcare Play Specialism Course was offered at:
- Bolton College
- Cardiff and Vale College
- North Warwickshire and Hinckley College
- Stanmore College
Mentoring training for working Healthcare Play Specialists was provided by HPSET.
In 2013 a small working group within the HPSET Board of trustees had developed a two-part workshop in response to issues and concerns arising from students undertaking the Foundation degree in Healthcare Play Specialism and healthcare play specialists who were their mentors. The one day workshop prepared registered practitioners for mentoring a foundation degree student regardless of whether they had a student assigned to them or not.
The second part a half-day session for the named mentors and students was integral to the college induction. This session introduced both parties to the competencies and HPSET requirements as set out in the Practice Assessment handbook at the commencement of the course.
2015
In 2015 the University of West London did not renew the contract with Stanmore College
due to the poor results of two Ofsted reports, related to their FE provision. At no time was the quality of the Healthcare Play Specialism provision in doubt. The last students completed their training in the summer of 2017.
Nescot College was approved in 2017 by the University of West London and started to deliver the course in February 2017.
The new Foundation Degree award was recognised as the requirement for application for professional registration with HPSET and a license to practice.

Suzanne Storer, upon her retirement as Chair of the Trust in 2015, set up the Suzanne Storer Profile of the Year award for the best profile of the year to support and encourage the enhancement of professional profiles audited as part of the re-registration process
2016
The HPSET website in 2016 was re-designed providing all registrants with a personal secure link to their own page on the register.
2018
In 2018 new legislation was introduced across Europe, The General Data Protection Regulation, HPSET undertook an intense review
and re-organisation of its policies, processes and practices, so that it was compliant with the new regulations.
In May2018 Tina Clegg, Chair of HPSET and Penelope Hart-Spencer, Chair of NAHPS formally wrote to the Health Professions Council (HCPC) seeking membership for the profession. We were informed that an act of Parliament had closed access to the HCPC. They advised that we consider an application to the Professional Standards Authority (PSA). A working party with representatives from HPSET and NAHPS has been established to investigate if an application to the PSA is viable.
FUTURE
Bolton College is due to merge with the University of Bolton in the spring of 2018.
They formally notified the University of West London in the autumn of 2017 that they would no longer be running the Healthcare Play Specialist course. They recruited their last intake in September 2017 and these students are due to complete their training in the summer of 2019.
HPSET and the University of West London are working to ensure that training opportunities continue. A Higher Apprenticeship framework is being developed as a result of the funding levy.
A public register accessed through the HPSET website will be introduced to promote public safety and professional registration in September 2018
In April 2018 HPSET Board approved the plans for GDPR compliance the move to annual reregistration for implementation in September 2018. The Nursing & Midwifery Council’s permission has been sought to adapt their revalidation process for Healthcare Play Specialist.
